Ensuring Safe Use of Energy
Early electrosurgical units (ESU) were grounded units. This meant that the electrical energy was delivered to the patient from the generator and returned to the ground. Since electricity always takes the path of least resistance, patients were at an elevated risk for burns as the energy sought the quickest route to the ground. (That could have been through an IV pole that inadvertently was touching the patient’s hand, for example.
Today’s ESU devices have been designed to force the electricity to return to the generator. This means the energy must flow through the patient and return through a dispersive electrode (grounding pad) or return through the other side of a bipolar device to the generator. As a safety mechanism, If the generator does not receive the energy back, it will stop functioning.

Dispersive electrodes return pads or grounding pads are a wonderful way to ensure that energy leaves the patient in a specified route; however, they are not without risk. Pad site burns can occur if the perioperative team is not careful. Dispersive electrode monitoring is a technology where the generator ensures that the grounding pad has adequate contact with the patient’s skin to decrease the risk of a burn.
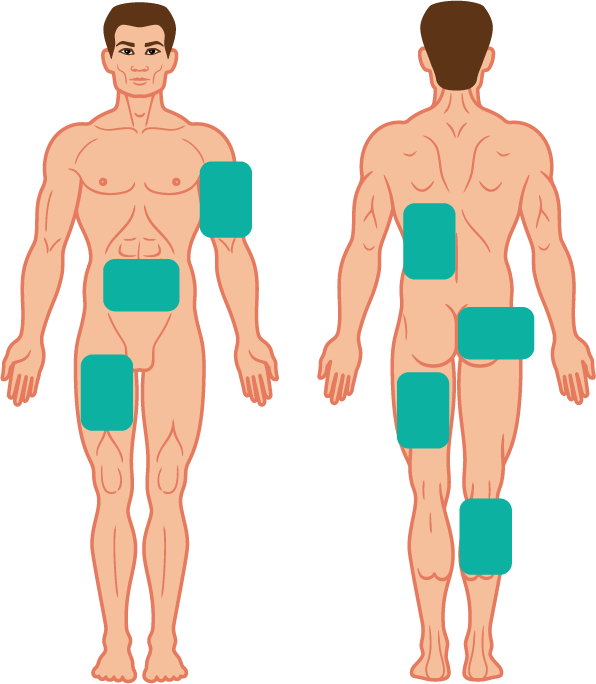
When placing a grounding pad, the following precautions must be taken. The site for the grounding pad must be:
- Well vascularized — energy travels easier through vascular tissue such as muscle.
- As close as possible to the surgical site to limit the energy movement within the patient.
- Placed flat and securely. Hair removal may be required to ensure a secure fit. If any part of the pad lifts off the patient, the surface area of the energy removal is decreased and places the patient at higher risk of burn.
Use advanced technology such as dispersive electrode monitoring when possible. Dual foil pads allow the generator to ensure good contact before allowing the unit to function.
(Ball, 2019)
What to do When you Cannot Place a Dispersive Electrode Monitoring Pad
Capacitive dispersive pads are great options for patients who have experienced large burns or have fragile skin, such as those with skin disorders, neonates or gerontological.
These are large reusable pads that are placed on the OR table. The patient lies directly on top of the pad, or a thin drawsheet can be placed in between. Using the technology of capacitation, the surgical energy flows from the patient into the pad and back to the ESU.
Patients Who Have Implanted Electronic Devices
Part of the preoperative assessment includes inquiring as to whether a patient has any implanted electronic devices. This could include a pacemaker, defibrillator, nerve stimulator, or other implants such as an insulin pump or cochlear implant. An implant could cause energy to pass through the device and damage it or cause it to malfunction.
(ORNAC, 2021)
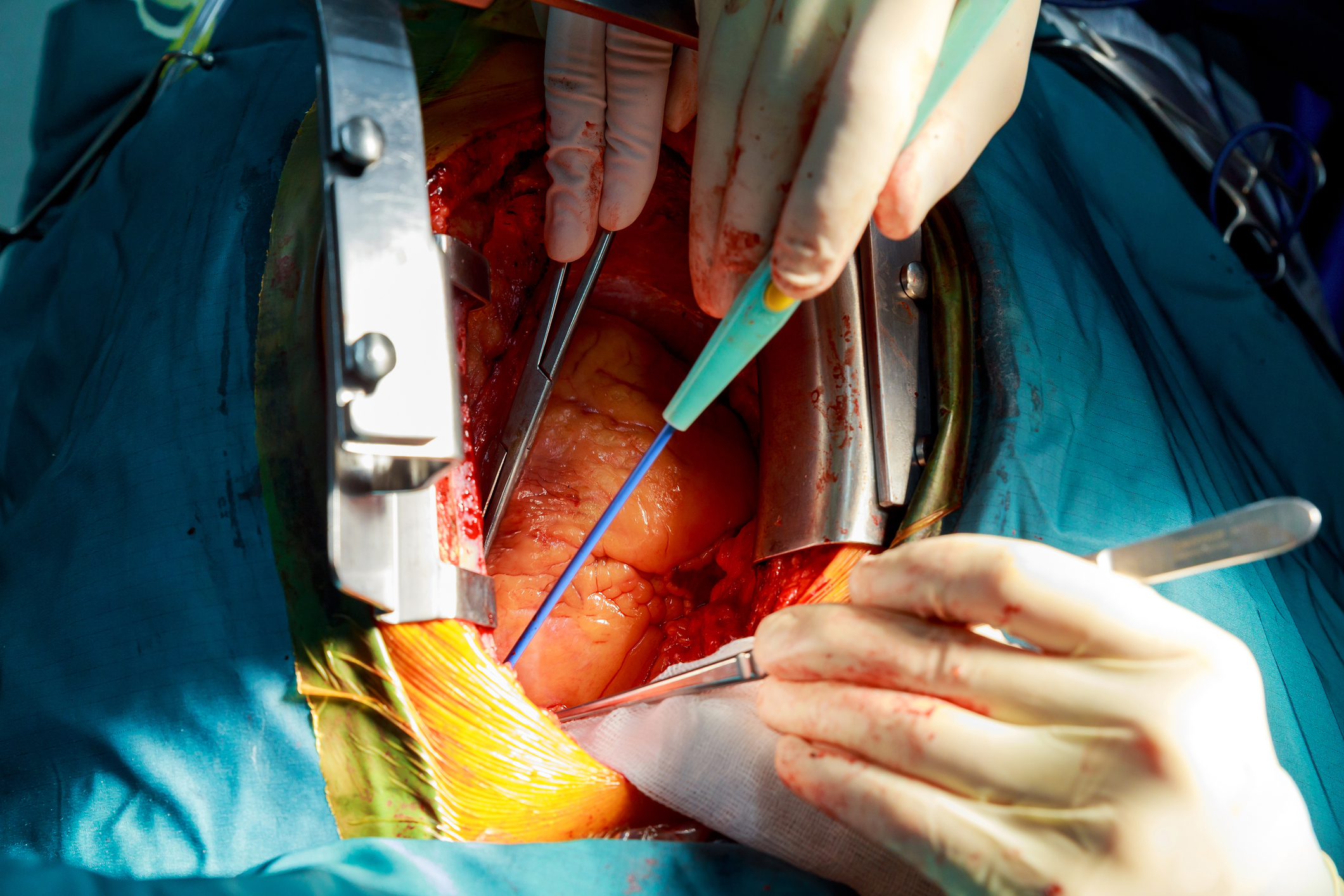
Direct Coupling: This occurs when an electrosurgical device is activated and accidentally touches a metal instrument that is not insulated. The energy can flow up the metal instrument and cause a burn to any tissue touching the instrument that is not protected or can cause a spark. This can also happen if the surgeon activates the electrosurgical device and touches a metal clip resulting in a burn.
To avoid this, surgeons must only activate an electrosurgical device once they have the target tissue in proximity.
(select the + hotspots in the image to reveal information)

Insulation failure
Laparoscopic instruments have a coating to insulate them, protecting tissue that may contact the shaft of the instrument when using electrosurgical energy.
If the coating is cracked or nicked, this can expose metal within the shaft. When electrosurgical energy travels down the shaft, it takes the quickest path to be grounded which could mean exiting the exposed metal on the shaft and causing a burn.
Because of the increased risk of internal burns, it is vital to inspect laparoscopic instruments to ensure the protective insulation layers are intact and no damage to the outer coating is present.